By Spencer Cramer, NCL Health Policy Intern
By Spencer Cramer, NCL Health Policy Intern
Spencer is a student at Brandeis University, where he is studying Politics and Health: Science, Society & Policy.
The COVID-19 pandemic has fostered a better understanding of how a public health emergency can devastate different groups of Americans already negatively impacted by health problems. These health disparities, which are differences in health outcomes based on factors such as race, ethnicity, or socioeconomic status, are deeply influenced by “social determinants of health.” Social determinants of health are factors in our environments and societies that have a large impact on someone’s health status, independent of their personal choices or lifestyle.
These social factors are the main contributors to health disparities, which represent one of the ugliest faces of inequality in America today. An example of how social determinants of health and health disparities are inextricably linked can be seen in the maternal mortality crisis, where Black women are more than three times more likely to experience a pregnancy-related death than white women. This disparity can be attributed to institutional racism, lack of access to maternal health services, and the aggregate stress of dealing with discrimination on a daily basis.
Even more illuminating, one of the best predictors of health outcomes is a person’s zip code. In many major U.S. cities, the gap in life expectancy between the highest and lowest zip codes is 20+ years. Similar gaps can be seen between different cities and states. Additionally, it is clear that locations with predominantly low-income populations and many people from racial or ethnic minority groups generally experience worse health outcomes than wealthier, white areas. Geographic location is an excellent predictor of health status for a couple of reasons. Our society still has a tremendous amount of segregation, as people of the same race, ethnicity, and socioeconomic background tend to live near each other. This means that the health inequities facing these groups become disproportionately concentrated in certain neighborhoods.
Another reason for these geographic health disparities is how under-resourced the physical neighborhoods are. Poorer and heavily minority neighborhoods are less likely to have parks, green spaces, quality grocers, and health services, and they are more likely to be afflicted by environmental pollution and other societal abuses. Urban planning has a huge impact on public health. Ensuring that we build our cities to equitably distribute public services and amenities will be a critical strategy in addressing social determinants of health and eliminating health disparities.
One way to create healthier communities for all would be to increase the amount and quality of green spaces like parks or urban forests. A large body of research suggests that urban green spaces provide a wide variety of health benefits to residents ranging from increased opportunities for exercise, cleaner air, and improved mental well-being. Urban trees are proven to be particularly important for removing pollutants and addressing other environmental risks, while improving many different health outcomes. Unfortunately, green spaces, parks, and urban trees are concentrated in whiter, richer, and healthier neighborhoods. Investing in parks and green urban spaces in disadvantaged communities can go a long way towards boosting health outcomes and increasing economic opportunities for those residents.
Perhaps nothing is more important for a community’s health than access to quality, nutritious, and affordable food. Unfortunately, millions of Americans live in food deserts, areas where there is little supply of nutritious, whole foods. Again, food deserts predominate poorer neighborhoods and racial and ethnic minority communities. Living in a food desert means that people cannot access healthy or substantial food at an affordable price, inadvertently resorting to more expensive, lower nutrition food from places like convenience stores. Poor diets driven by this lack of food access cause tons of health problems and are a key driver of health disparities. As a society we often associate diet with personal choice. However, people living in food deserts usually have no option other than to eat low-quality food, and subsequently suffer from the health consequences. Ensuring that all neighborhoods and communities can easily access healthy food at affordable prices will surely help to reduce disparities in areas such as obesity, diabetes, heart disease, and others. What we eat everyday has an astronomical impact on our health, so we must make equitable access to good food a priority when creating healthier communities.
Similarly, many of the same neighborhoods plagued by food deserts also suffer from a stunning lack of access to health and medical services. Many healthcare resources are *concentrated in areas with higher insurance rates, especially places with high rates of private insurance, leaving neighborhoods with many uninsured or Medicaid-eligible residents without needed health providers. The health consequences caused by the uneven distribution of health services can be devastating and can result in the delay in crucial preventive health screenings. To address this, we can provide incentives, like additional funding or student loan forgiveness to health care providers who practice in underserved communities, and implement public policies to achieve an equitable geographic distribution of medical resources.
A final factor that leads to these health inequalities between zip codes is pollution. It is certainly no secret that environmental pollutants are often horribly damaging to human health. They can cause diseases ranging from asthma to cancer, and are devastating for any community that they afflict. And of course, pollution has a disparate impact on lower-income and predominately minority communities. Developers frequently choose to build factories and other waste-producing sites in these communities because their residents have fewer resources and less political and social capital to advocate against them. Nobody should be subjected to residing in the midst of toxins and waste.
This will require a massive shift to clean energy, responsible development, and safer waste disposal. We can create more health equity by eliminating the health costs brought upon poor and minority communities by pollutants. Designing our neighborhoods and cities with a focus on public health and health equity will help to close the gaps in health outcomes between different zip codes, and should be one of our top priorities as we battle health disparities and social inequities.
*Links are no longer active as the original sources have removed the content, sometimes due to federal website changes or restructurings.



 By Spencer Cramer, NCL Health Policy Intern
By Spencer Cramer, NCL Health Policy Intern
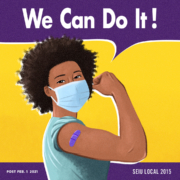
 By Guest Blogger April Verrett, President of SEIU 2015
By Guest Blogger April Verrett, President of SEIU 2015