The eleventh annual Script Your Future contest saw participation by 24 schools in 11 states and directly counseled nearly 7,000 patients nationwide
Media contact: National Consumers League – Katie Brown, katie@nclnet.org, (202) 207-2832
May 13, 2022
Washington, DC —Today, the National Consumers League (NCL) and its partners announced the winners of the eleventh annual Script Your Future Medication Adherence Team Challenge, a competition designed to engage pharmacy students and faculty across the nation by encouraging teams to develop creative initiatives to raise public awareness about the importance of medication adherence, vaccine confidence, and safe drug disposal.
This year’s winners are Wilkes University, Temple University, Western University, Northeast Ohio Medical University (NEOMED), University of Pittsburgh, and Touro University California.
The 2022 Script Your Future Team Challenge is an awareness campaign coordinated by NCL with support from its partners and the Challenge sponsors—Eli Lilly, Deterra, the American Association of Colleges of Pharmacy (AACP), the American Pharmacists Association (APhA), and the National Community Pharmacists Association (NCPA).
The Team Challenge was first established in 2011 to nurture adherence-minded values in future generations of professionals entering the workplace.
In 2022, our Team Challenge student health professionals spread messaging on the importance of medication adherence, vaccine confidence, and a new health topic: safe drug disposal. This year, over 1,000 future healthcare professionals and volunteers from across 11 states participated in the Team Challenge.
2021 Medication Adherence Team Challenge Winners
This year’s winners, selected from dozens of applications and 24 participating educational institutions, are listed below.
National Award Winner: Wilkes University Nesbitt School of Pharmacy – PA
Wilkes University is a fourth-time participant of the Script Your Future Team Challenge, and a first-time winner of the National Award! During the 2022 Team Challenge, students on the Wilkes team successfully collaborated with Highmark Health pharmacists to create a medication adherence questionnaire that was circulated to patients. They also creatively used social media, including TikTok and YouTube, to spread messages about the importance of medication adherence, vaccine confidence, and safe drug disposal. These messages got over 58,000 views. Students were also able to vaccinate patients for COVID-19 (boosters), Shingles, and Influenza. The Wilkes team was able to directly counsel 1,184 patients, and reached 49,313 people through their outreach efforts.
National Award Winner: Temple University School of Pharmacy – PA
Temple University is also a first-time winner of the Script Your Future National Award! This year, Temple students of pharmacy collaborated with health and community organizations in Philadelphia, including Temple University Hospital, and its affiliated clinics as well as the places where people live their lives such as local community pharmacies, parks, churches, charitable organizations, and schools. For example, Temple’s team worked with Dispose Rx to spread messages about the importance of safe drug disposal in North Philadelphia. This team also worked with the Children’s Mission to serve people who have no or unstable housing, and counseled them on their medications along with conducting blood pressure checks. Temple students directly counseled 234 patients, and reached over 400 patients through their activities.
Health Disparities/Underserved Focus Award Winner: Northeast Ohio Medical University School of Pharmacy – OH
The Northeast Ohio Medical University School of Pharmacy (NEOMED) team is this year’s winner of the Script Your Future Health Disparities Award! NEOMED’s team focused on reaching low-income and homeless individuals, the elderly, and refugees. NEOMED students worked with the Center for Families and Children, IKON Health Foundation, and Rose Centers for Aging Well to reach these underserved populations. Through their efforts, the NEOMED team vaccinated 456 patients, directly counseled 1,323 patients, reached 1,923 patients, and distributed and donated 3,254 resources.
Media Outreach Award Winner: Western University School of Health Sciences, College of Pharmacy – CA
This year’s winner of the Media Outreach Award is Western University College of Pharmacy! This team implemented creative uses of traditional and social media to spread messaging related to medication adherence, vaccine confidence, cardiovascular disease, diabetes, interprofessional collaboration, antimicrobial resistance, and safe drug storage & disposal. They created a brand-new podcast series that aimed to provide information on these topics, and made them available on multiple media platforms including Spotify, Apple Podcasts, Google Podcasts, and their website. The podcast series can be found here. Across all of these platforms, Western University’s team was able to get 1,203 views.
Creative Interprofessional Team Event Award Winner: University of Pittsburgh School of Pharmacy – PA
University of Pittsburgh’s pharmacy students demonstrated great interprofessional collaborations with other health professional students at their university. Their team included students from the University of Pittsburgh’s School of Dental Medicine, School of Health and Rehabilitation Sciences, School of Medicine, School of Nursing, and School of Social Work. Their multi-disciplinary intervention with different health professional students helped to bring multiple perspectives and skills sets together to bridge gaps in expertise when counseling patients. Their interprofessional team documented over 1,800 unique patient encounters at community pharmacy sites, including patients with disease states like hypertension, diabetes, and dyslipidemia to transplant and neurologic disorders.
Technology Innovation Focused Award: Touro University California, College of Pharmacy – CA
Touro University’s pharmacy students implemented creative uses of technology to increase messaging for medication adherence. They created a digital medication adherence wallet card, to help patients keep track of their medications in a more convenient way. Given that technology is so widely used today, this was a great effort by the students. They did mention an important issue, that there are people who do not have internet access, so these digital cards were given in complement with the physical wallet cards.
2022 School
Congratulations to the winners of the 2022 Script Your Future Medication Adherence Team Challenge!
A word from NCL and one of our generous Script Your Future sponsors
“The Script Your Future program has been a great way to engage future health professionals and spread messages about the importance of medication adherence, vaccine confidence, and now, safe drug disposal. As we are still combatting the COVID-19 pandemic, it is important to keep patients on top of their health care needs, and participants of this program have been a part of these efforts. This year, we had over 1,000 participants conduct community outreach activities, and NCL continues to be impressed by the impact these students have on their respective communities across the country.”
- NCL Executive Director, Sally Greenberg
“Student pharmacists have been important contributors to the outreach to communities, especially throughout the pandemic. Medication adherence, vaccine access, and substance use prevention are critically important priorities and AACP appreciates NCL’s commitment to this recognition program.”
- American Association of Colleges of Pharmacy (AACP) Executive Vice President and CEO, Lucinda L. Maine, PhD, RPh
###
About the National Consumers League (NCL)
The National Consumers League, founded in 1899, is America’s pioneer consumer organization. Our mission is to protect and promote social and economic justice for consumers and workers in the United States and abroad. For more information, visit www.nclnet.org.
 By Sam Sears, Health Policy Associate, National Consumers League
By Sam Sears, Health Policy Associate, National Consumers League






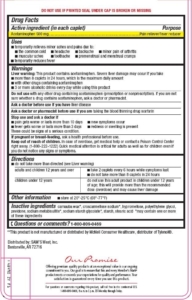 Consumer education is a key step to ensuring safe acetaminophen use and preventing overdoses. A new report from the Acetaminophen Awareness Coalition (of which National Consumers League is a founding member) “
Consumer education is a key step to ensuring safe acetaminophen use and preventing overdoses. A new report from the Acetaminophen Awareness Coalition (of which National Consumers League is a founding member) “
 There are more than 600 over-the-counter and prescription medications that contain acetaminophen making it the most commonly used drug ingredient in the United States. Acetaminpophen can be found in pain relievers, fever reducers, sleep aids, and cough, cold, and allergy medicine. It is especially important during cold and flu season to understand the dangers of mixing medicines.
There are more than 600 over-the-counter and prescription medications that contain acetaminophen making it the most commonly used drug ingredient in the United States. Acetaminpophen can be found in pain relievers, fever reducers, sleep aids, and cough, cold, and allergy medicine. It is especially important during cold and flu season to understand the dangers of mixing medicines.












